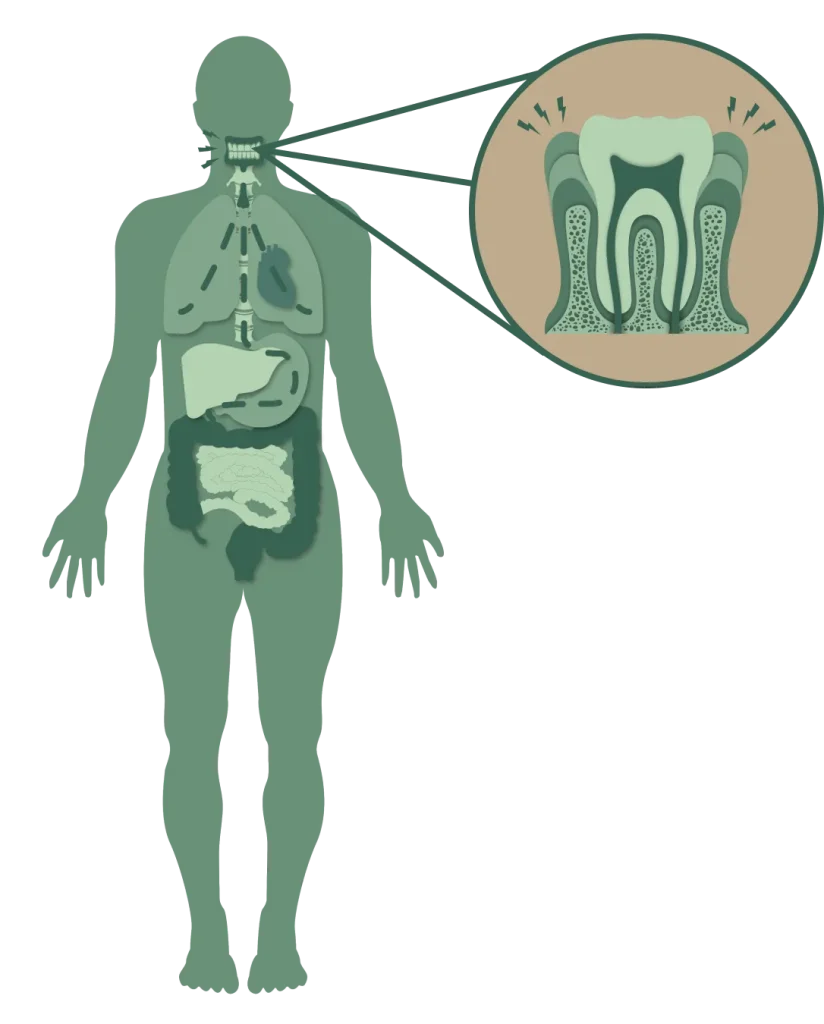
Hygiene has been the dominant model of oral health since the early 1900’s. It’s still relevant today – we need to help ensure that people have clean teeth. However, managing inflammation has become my go-to model in managing health. Here’s why- inflammation is one of the root causes of all disease, not just in your mouth, but in your whole body. If your gums are inflamed, your body is inflamed. It’s also clear that many people have oral inflammation despite having clean teeth. More hygiene won’t help this group. Luckily, we have some inflammation management tools that can help. In the scientific literature, many of these concepts fall under the heading of Periodontal Medicine.